Image credit: Steven Cornfield on Unsplash
Worldwide, 64 candidate COVID-19 vaccines are currently in clinical assessment, including 13 vaccine candidates at phase 3 and 173 vaccines are in preclinical analyses. Phase 3 candidate vaccines include a variety of vaccine platforms, such as vector vaccines, mRNA vaccines, inactivated vaccines, and adjuvanted recombinant protein nanoparticles.
An interim analysis of data from the phase 3 trial of the COVID-19 vaccine from Russia (Gam-COVID-Vac) suggests that a two-dose regimen of the adenovirus-based vaccine offers 91.6% efficacy against symptomatic COVID-19.
“Stopping the COVID-19 pandemic requires the introduction of different vaccines based on different mechanisms of action to cover diverse global health demands,” said Dr. Denis Logunov, co-lead author, Gamaleya National Research Centre for Epidemiology and Microbiology, Russia. “Our vaccine, along with other SARS-CoV-2 vaccines, helps to diversify the world SARS-CoV-2 vaccine pipeline.”
The preliminary findings, published in The Lancet, are based on analysis of data from nearly 20,000 participants, three-quarters of whom received the vaccine and one quarter received a placebo. Serious adverse events (those requiring hospital admission) were rare in both the placebo (0.4% [23/5,435]) and vaccine (0.2% [45/16,427]) groups and none were considered associated with vaccination.
In a comment published alongside the Lancet paper, Professors Ian Jones and Polly Roy said: “The development of the Sputnik V vaccine has been criticized for unseemly haste, corner-cutting, and an absence of transparency. But the outcome reported here is clear and the scientific principle of vaccination is demonstrated, which means another vaccine can now join the fight to reduce the incidence of Covid-19.”
They pointed out the vaccine had good effect in all age groups, including in patients 60 years and older, and reduced the seriousness of the disease after one dose. This was “particularly encouraging” while supply of the vaccine is limited, they added.
Two different vaccines doses
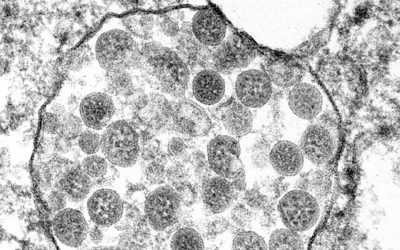
The Gam-COVID-Vac is a two-part vaccine that includes two adenovirus vectors — recombinant human adenovirus type 26 (rAd26-S) and recombinant human adenovirus type 5 (rAd5-S) — which have been modified to express the SARS-CoV-2 spike protein. Adenoviral vector vaccines are commonly used in flu vaccine development, and their safety has been confirmed in several clinical studies.
In cases of vaccine use, the adenoviruses are weakened through genetic manipulation so that they cannot replicate in human cells or cause disease. They also have the added benefit of not requiring the same frigid storage temperatures as the mRNA vaccines developed by Pfizer and Moderna, which could bring down its cost and facilitate transportation and storage.
In this trial, participants were given one dose of rAd26-S followed by a booster dose of rAd5-S 21 days later. The study’s authors explain that using a different adenovirus vector for the booster vaccination may help create a more powerful immune response compared with using the same vector twice, as it minimizes the risk of the immune system developing resistance to the initial vector.
“Our interim analysis of the randomized, controlled, phase 3 trial of Gam-COVID-Vac in Russia has shown high efficacy, immunogenicity, and a good tolerability profile in participants aged 18 years or older,” said Dr. Inna Dolzhikova, co-lead author, Gamaleya National Research Centre for Epidemiology and Microbiology, Russia.
Encouraging results
Between September 7 and November 24, 2020, a total of 21,977 adults were randomly assigned to receive the Gam-COVID-Vac vaccine (16,501) or placebo (5,476), which was administered in two doses. PCR tests to detect infection with SARS-CoV-2 were done at screening and at dose 2 (given after 21 days). From 21 days after receiving the first dose, 16 cases of symptomatic COVID-19 were confirmed in the vaccine group (0.1% [16/14,964) and 62 cases (1.3% [62/4,902]) in the placebo group — equivalent to an efficacy of 91.6%.
The vaccine was shown to induce a robust humoral response (also called antibody response) and cellular immune response (also called T-cell response) with data from 342 and 44 participants, respectively. Six of the 342 vaccinated participants did not mount an immune response following vaccination, which the authors attribute to their age or individual responses of their immune systems.
The authors note that because COVID-19 cases were detected only when participants self-reported symptoms (followed by a PCR test), the efficacy analysis only includes symptomatic cases of COVID-19, and further research is needed to understand the efficacy of the vaccine on asymptomatic COVID-19, and transmission. Furthermore, patient follow up was done on average at 48 days from the first dose, so the study cannot yet make any conclusions with regards to the duration of protection.
Racial representation was also limited in this preliminary phase as most participants in the trial were white, so further research will be needed to confirm the results in a more diverse group of participants. Although the study enrolled participants with comorbidities, not all risk groups were represented.
In addition, the authors report a need for further research to investigate the vaccine in adolescents and children, as well as pregnant women. The trial is ongoing and aiming to include a total of 40,000 participants — monitoring of safety and efficacy continues.
While the vaccine was initially met with criticism, perhaps these interim results provide some justification for the hasty implementation of the vaccine prior to completion of the Phase 3 study, given the unprecedented circumstances posed by the pandemic.
Dr Julian Tang, a clinical virologist at the University of Leicester, said in an interview with the BBC: “Despite the earlier misgivings about the way this Russian Sputnik V vaccine was rolled out more widely — ahead of sufficient Phase 3 trial data — this approach has been justified to some extent now.
“Such pandemic-related vaccine rollout compromises have, to be fair, been adopted in the UK vaccination programme also — with the extended intervals between the first and second doses. So we should be more careful about being overly critical about other countries’ vaccine designs.”
Whether or not the ends justify the means is still up for debate, but even in unprecedented situations, lowering standards or circumventing protocols that ensure public safety are dangerous precedents to set that not only put lives at stake but can harm public perception of these processes.
Reference: Denis Logunov, et al., Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia, The Lancett (2021). DOI: 10.1016/S0140-6736(21)00234-8