The most common and deadly form of adult brain cancer, glioblastoma (GBM), rarely metastasizes outside of the central nervous system. Instead, the tumor cells invade into the brain itself, causing disruption in brain circuits, blood vessel and flow changes, and swelling. Most patients succumb to this disease in less than 15 months even with the most aggressive treatments, which often come with devastating neurological consequences.
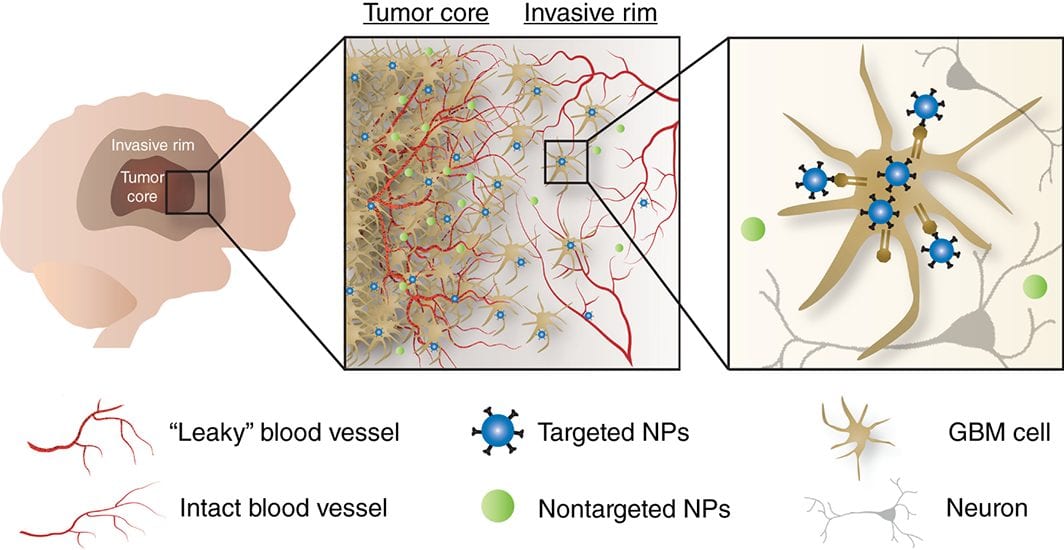
Passive versus active tumor targeting.
Current treatments include maximal surgical removal when safe and feasible, followed by radiation and oral or local interstitial chemotherapy to address the residual, invading tumor cells. However, delivering effective and sustained treatments to these invading cells without worsening damage to the adjacent brain is a major challenge and focus of the emerging fields of nanomedicine and viral- and cell-based therapy. Numerous groups have studied and engineered therapeutic and/or diagnostic nanoparticles to specifically target brain-invading tumor cells. This approach offers the potential to significantly increase therapeutic efficacy while minimizing toxicity and off-target effects. In addition, this particle-based formulation approach allows flexibility in changing the therapeutic agent(s) and/or combining various therapeutic agents to tailor the treatment strategy to individual patient tumors in future applications.
A recent review by Aniket S. Wadajkar, Jimena G. Dancy, David S. Hersh, Pavlos Anastasiadis, Nhan L. Tran, Graeme F. Woodworth, Jeffrey A. Winkles, and Anthony J. Kim from the University of Maryland School of Medicine summarizes the main barriers to effective GBM patient therapy and describes recent progress related to GBM tumor cell-targeted nanotherapeutics. Read it in WIREs Nanomedicine and Nanobiotechnology.