Cancer treatment, specifically whether the immune system recognizes and attacks cancer, had been discussed for over 100 years. The debate, however, is settled and the conclusion is that it does recognize and attack cancers by the mechanism of immunosurveillance, but some cancers manifest local immune suppression and resist the immune attack.
Now that this debate over, the focus has appropriately shifted to identifying the most effective immunotherapies for cancer, which use the patient’s own immune system to attack cancers anywhere in the body, and bringing them through clinical trials into usage. One key to successful immunotherapy is disrupting the immune suppressive mechanisms mediated by the cancer that repress the ability of our natural immune system to recognize and fight off cancer.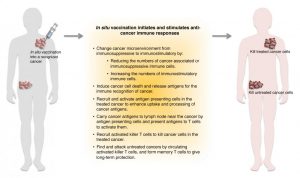
Most cancer therapeutic approaches are of limited value against the majority of malignant/metastatic cancers, which require systemic therapy. Chemotherapy has been the only modality that can treat metastatic disease, but all too often, chemo-resistance develops and the patient dies from metastatic cancer.
Perhaps not surprisingly, the focus has been on using immunotherapy like chemotherapy is used, by systemic administration, which can be effective in a minority of patients, and is often limited by toxicity. For example, the most established immunotherapies, such as systemic cytokine delivery and systemic immune checkpoint blockade antibody therapy, still are unable to improve outcomes for many patients due to its toxicity and severe immune-related adverse effects from systemic administration.
Putting immunostimulatory reagents into a recognized cancer can generate effective systemic anti-cancer immunity by breaking the local immunosuppression, which is a main accounting issue of current immunotherapies, and stimulating local immune attack on the cancer.
This strategy is “in situ vaccination” in which the cancer itself serves as the antigen and the treatment applies immunomodulatory adjuvant. The local treatment of an adjuvant as an in situ vaccination can modify the immune suppression that dominates the cancer microenvironment to an immunostimulatory environment that enables the immune recognition of the cancer to proceed and attack the cancer. When optimally done, a robust local anti-cancer immune response induced by this approach can also generate long-lasting systemic immune protection and impacts metastatic cancers.
The advantages of in situ vaccination are: simple and cost-effective; less toxicity and minimal systemic side effects; feasible and flexible adjuvant delivery; exploiting all cancer antigens already in the cancer avoids the need to identify antigens; utilizing all antigens in the cancer minimizes immune escape; and potential synergy when combined with other therapies, such as radiation, hyperthermia, nanotechnology, and other immunotherapy.
Read more in a recent review article in WIREs Nanomedicine and Nanobiotechnology.
Kindly contributed by the Authors.-

















