The eye is a sensory organ consisting of compactly adjoined tissues that are arranged as a globular structure known as the eye ball. All the tissue structures of the eye function together to enable vision. The structure and function of the eye is affected in pathological conditions, thus demanding therapeutic interventions. These interventions majorly involve treatment with therapeutic agents, such as drugs/bioactive molecules. The therapeutic agents, in the form of a suitable formulation (such as solution, suspension, or ointment), are administered to ocular tissues either as topical eye drops (non-invasive) or as intraocular injections (invasive).
Due to the presence of physical (cornea, conjunctiva, sclera, and retinal pigmented epithelium) and physiological (tear fluid, aqueous humor, and choroidal blood circulation) ocular barriers, the bioavailability of topically or intraocularly administered medicaments is reduced, thereby demanding frequent drug administration. Frequent drug administration using invasive intraocular injections can cause intraocular bleeding accompanied with pain and discomfort that results in poor patient compliance. Therefore, delivery systems that can improve bioavailability and retention time of drugs in ocular tissue can potentially provide therapeutic concentrations for optimal durations, and hence enable effective treatment of eye diseases.
Nanoscale drug delivery systems, or nanomedicines, have revolutionized the field of ocular drug delivery by offering improved bioavailability of topically/intraocularly administered therapeutic molecules compared to conventional formulations.
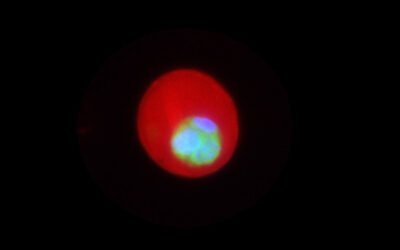
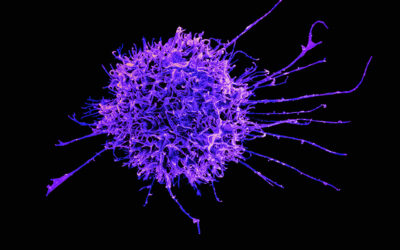
Nanoparticles—one of the important carrier systems used in nanomedicine—are colloidal drug delivery systems that facilitate permeation of the entrapped therapeutic agents across ocular tissues. Nanoparticles can not only improve residence time of entrapped cargo molecules, but can also sustain the release of the drug over longer durations, helping to reduce the frequency of drug administrations. Nanomedicines therefore have the potential to treat ocular diseases more effectively.
Prof. Dhirendra S. Katti’s group from the Indian Institute of Technology Kanpur discuss the important physicochemical characteristics of nanoparticulate drug delivery systems (such as liposomes, polymeric nanoparticles, microemulsions, nanosuspensions, dendrimers, micelles, solid lipid nanoparticles, nanostructured lipid carriers, niosomes, and cubosomes) in governing nanoparticle–tissue interactions, ocular retention, and bioavailability of topically/intraocularly administered therapeutic agents, in an article in WIREs Nanomedicine and Nanobiotechnology. They infer that understanding the interaction, permeability, and partitioning of delivery systems in ocular tissues can help design delivery systems with improved retention time and bioavailability.
Kindly contributed by the Authors.