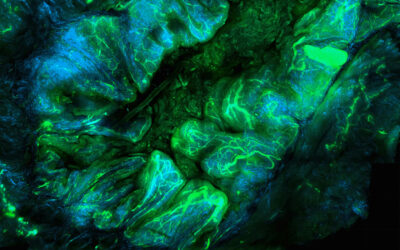
Image credit: Mayo Clinic
Transcatheter embolization is a minimally invasive procedure in which medications or synthetic materials — also referred to as embolic agents — are placed through a catheter to block blood flow to specific areas in the body. They are commonly used to control or prevent abnormal bleeding, treat aneurysms, or close off blood vessels that supply blood to a tumor.
A variety of embolic agents, such as coils, beads, and liquid agents, are currently being used in life saving treatments. However, there are risks associated them such as possible reopening of the occluded pathway, long-term toxicity, risk of nonspecific embolization, and possible stroke.
Another challenge lies in the fact that the nature of vascular diseases requires that embolic agents be versatile. “Clinical scenarios can require the occlusion of blood vessels ranging in size from arteries (up to 1–2 cm diameter) to capillaries (5–10 μm diameter),” said Dr. Rahmi Oklu M.D., Ph.D., and researcher at the Mayo Clinic.
“The decision to use clinically available embolic agents highly depends on the size and geometry of the targeted vasculature,” he continued. “Therefore, the efficacy of an embolic agent is dependent on its ability to adapt to unique clinical scenarios presented by each patient and its ability to deliver effective treatment while minimizing any side effects.”
In a recent study published in Advanced Materials, a team led by Oklu sought to overcome these drawbacks using malleable hydrogels, which according to the researchers, offer significant advantages over both solid and liquid embolic agents currently being used in the clinic.
“[The goal] is to develop innovative embolic agents that have the ability to adapt to unique cases presented by each patient, as well as possess desirable mechanical, radiopaque, and biological properties for effective treatment while also minimizing collateral injury to adjacent tissues,” said Oklu.
To do this, Oklu and his team developed a unique class of material derived from an extracellular matrix (ECM)‐based hydrogel. In recent years, injectable ECM hydrogels have been used with positive outcomes in non-invasive procedures involving tissue repair and organ replacement. “The strategic design of this malleable gel enables it to be delivered using most clinical catheters, and it forms an impenetrable solid cast of the vessel geometry, avoiding embolization failure and recurrent bleeding,” said Oklu.
“The current paradigm for embolization is to achieve an occlusion only; our aim is to challenge this with the next generation embolic agents that are bioengineered not only to occlude the vessel, but also to modulate the biology of the occluded vessel to promote healing, deliver drugs and therapeutics.”
To create their regenerative hydrogels, the team isolated extracellular matrix — the non-cellular component of tissue that provides physical scaffolding to cells — from swine cardiac tissue through a process called decellularization, in which cells are removed leaving behind the ECM scaffold. “Cardiac ECM was selected because it can promote muscle regeneration, facilitate vascularization, and modulate macrophage polarization toward tissue healing without hemocompatibility issues,” said Oklu. “These properties suggest that cardiac ECM is biocompatible and regenerative, which can be highly beneficial for the remodeling of embolized diseased vessels.”
The collected ECM was pulvarized and combined with laponite nanoclay to create the hydrogel. “The design of ECM–nanoclay hybrid nanocomposites integrates the biochemical and biomechanical cues from the ECM and the mechanical strength from synthetic nanoclay to promote constructive remodeling in embolized arteries,” said Oklu.
The flexible and healing hydrogel is easy to deliver in most clinical catheters, and forms an impenetrable solid cast of the desired blood vessel’s natural shape and geometry, not only promoting healing but also avoiding embolization failure and recurrent bleeding. “It provides the versatility and efficacy that cannot be achieved by clinically used embolic agents,” added Oklu.
The new embolic hydrogel can also be retrieved if off-site embolization is observed, something that is not possible with coils or other liquid embolic agents. Medical practitioners can retrieve the gel using an aspiration pump, which will great improve treatment safety. The gel is also biodegradable, and is gradually replaced with fibrotic tissue, which according to Oklu, leads to a durable occlusion of the embolized vessels. “In other words, the gel will be eventually eliminated from the body naturally after accomplishing its function,” he said.
“We aim to further the engineered gel embolic agents to deliver therapeutics, including cells, drugs, gene therapy and viral vectors. Longer survival studies will be performed to investigate the material’s embolic efficacy in the long term.”
Reference: Jingjie Hu, et al., Bioactive‐Tissue‐Derived Nanocomposite Hydrogel for Permanent Arterial Embolization and Enhanced Vascular Healing, Advanced Materials (2020). DOI: 10.1002/adma.202002611

![OkluGel1_49[1]](https://www.advancedsciencenews.com/wp-content/uploads/2020/09/OkluGel1_491.jpg)