One of the most challenging steps when developing a new drug is to have it reach the desired location in the body, be it an organ or a specific cell type.
For diseases that affect the lungs, the obvious delivery method would be inhalation, but in some cases, such as pulmonary fibrosis — a disease that affects the alveoli in the lungs and causes shortness of breath — this can be easier said than done.
Nintedanib is a drug that has been found to be very helpful for its treatment, but when inhaled, it is rapidly diffused to the bloodstream and does not have enough time to act where it’s needed.
A study led by scientists from the University of Pennsylvania showed how the use of nanocarriers improves nintedanib retention and distribution in lung cells after drug inhalation. In particular, in the lung’s alveoli, which are small air sacs that allow the exchange of gases, such as oxygen and carbon dioxide, between the lungs and the blood, and which are primarily affected in pulmonary fibrosis.
“We loaded nintedanib into [liposome] nanoparticles to deliver it directly to the lung in a highly concentrated form,” said Laura Ferguson, a pulmonary and critical care fellow in the Department of Medicine, Pulmonary, Allergy, and Critical Care Division of the University of Pennsylvania, Philadelphia, US, and first author of the study. “This work is important for potentially changing how the drug is taken by patients.”
Dodging whole-body drug distribution
At the moment, patients with pulmonary fibrosis are prescribed oral nintedanib to help slow down disease progression. When a drug is taken orally, it reaches the bloodstream and distributes throughout the whole body.
This means a high concentration is needed for the drug to have an effect on the desired organ. But when a large amount of drug is taken, it usually correlates with undesired side effects or even toxicity. If the drug concentration is decreased, the side effects are diminished, but the drug becomes less effective.
This often occurs in cases of pulmonary diseases, according Ferguson, and “nintedanib [is] a drug that doctors use to treat pulmonary fibrosis but has side effects that limit how well it can work.”
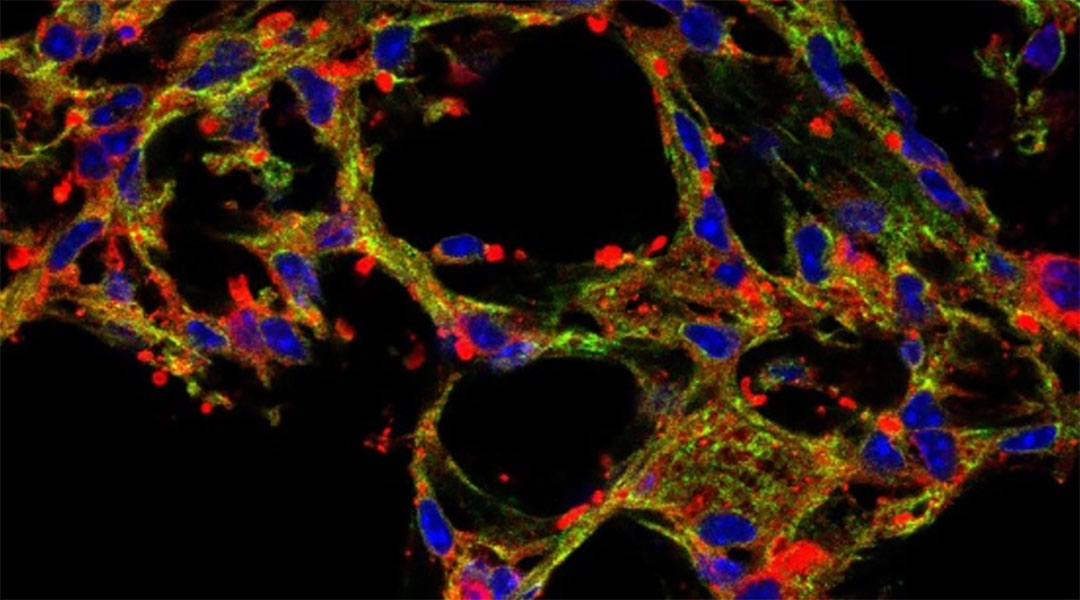
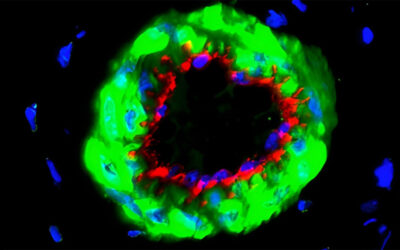
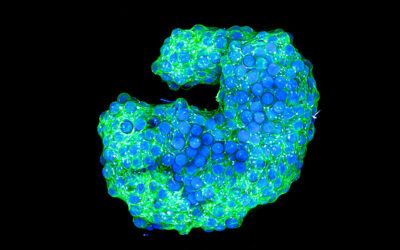
Ferguson and the team decided to develop a new, more direct way of delivering the drug to the alveoli at higher concentrations while avoiding undesired toxicity. To do this, the team loaded nintedanib into liposome structures, which are tiny, spherical “bubbles” with a lipidic shell and an inner aqueous core where the drug is concentrated.
To test the delivery method, the scientists introduced the drug-loaded liposomes into the airways of mice and monitored the arrival and retention in the alveoli.
The team observed that liposomes loaded with the drug remained in the lung’s alveolar structures for at least 20 hours, potentially giving the drug enough time to work on its target. In addition, they checked for their distribution in the body and observed that the liposome concentration in the blood, stomach, liver, and spleen was very low, suggesting that nanoparticle inhalation of nintedanib could avoid undesired side effects.
Liposome nanocarriers for lung diseases
The most exciting finding was that with this methodology, nintedanib remains in the lungs ten times longer than oral intake, the current standard of care. With this promising data, the team plans to test it in a mouse model of pulmonary fibrosis and evaluate its performance in treating the disease and confirming lowered toxicity when compared with oral nintedanib.
The team does not want to stop at nintedanib and pulmonary fibrosis though. “We are excited to continue to develop this drug delivery system for other small molecule drugs and for RNA delivery,” Ferguson added.
This includes treatment of other alveolar diseases, such as pneumonia, acute respiratory distress syndrome (ARDS), and COVID-19-derived pneumonia, to help develop better therapeutic options.
“Many drugs have dose-limiting side effects or such severe side effects that they cannot be taken at all by humans,” said Ferguson. “If drugs can be delivered in a more targeted fashion, like by directly inhaled nanoparticles, treatment for many lung diseases could be improved.”
Reference: Jacob S. Brenner, et al., Mechanisms by which liposomes improve inhaled drug delivery for alveolar diseases, Advanced NanoBiomed Research (2023). DOI: 10.1002/anbr.202200106