Researchers have developed a miniature intestine-on-chip to elucidate inflammatory mechanisms and test an existing therapy for inflammatory bowel disease.
Even as inflammatory bowel disease affects millions of people around the world, its underlying causes remain undefined, which means most available therapies target symptoms, with many patients not always responding well to treatment.
While researchers employ a myriad of models to understand its underlying mechanisms and test suitable therapies, they all suffer from various issues. Better models are needed to understand how inflammatory bowel disease develops.
“In recent years, intestine-on-chip systems have proven their relevance for modeling inflammatory bowel disease in [lab studies], as it is possible to build the systems component by component and to reproduce the biological complexity needed for [this] research,” said Oanh Nguyen, a researcher at ETH Zurich and first author of the study, in an email.
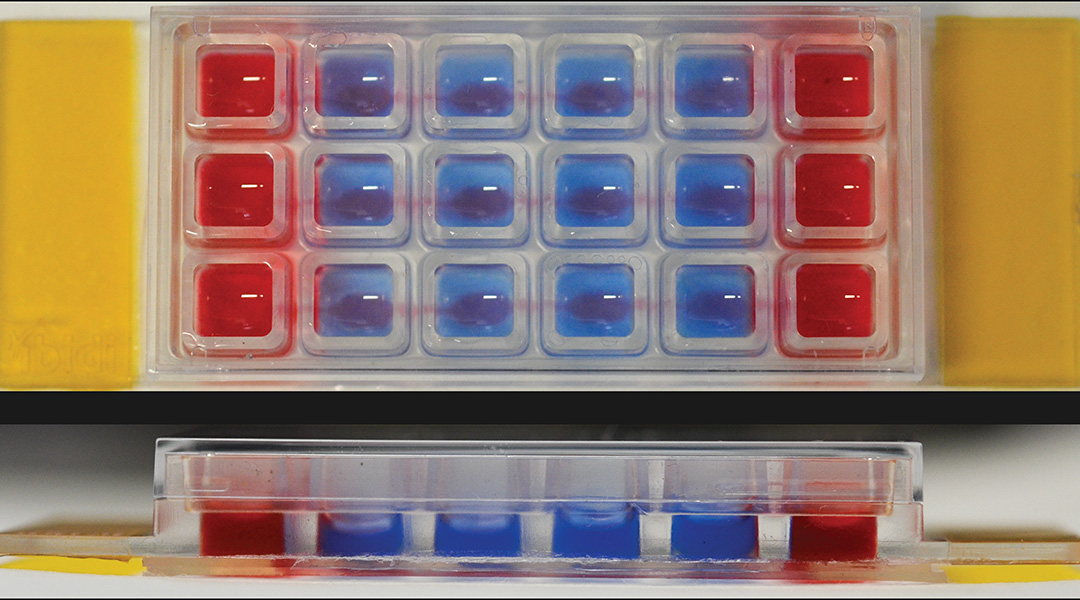
Often, problems with the materials, their fabrication, and the extensive setup and expertise required can make these systems impracticable. To solve this, Nguyen and colleagues crafted a thermoplastic microfluidic chip about the size of a standard microscopic slide (25 mm by 75 mm in size), with multiple wells. This chip has multiple channels and compartments fashioned in a manner that allows liquid to flow between the different sections.
Building an artificial gut
To replicate the microenvironment found in the intestine, they sequentially cultured the most common types of cells found in the intestinal lining on a collagen scaffold within the wells. Whether a dysfunctional intestinal lining causes inflammatory bowel diseases or arises due to the condition is still uncertain, and the team hope models such as this can help find an answer.
After seven days, the researchers had established a functional layer of cells that represented the intestinal barrier in a compact setup. Using microscopic and analytical techniques, they were able to confirm the presence of the intestinal barrier.
Once they had successfully created this set up, the team instigated inflammation — often observed in inflammatory bowel disease — in the cellular model within the chip. They added various immune cells and inflammation-inducing molecules to the different wells, and observed the triggering of inflammation.
Next, the researchers sought to demonstrate the chip’s ability to act as a testing ground for anti-inflammatory therapies. For these experiments, they began by inducing inflammation after 24 hours, added Infliximab, a drug approved to treat several autoimmune conditions, including two that are inflammatory bowel diseases — Crohn’s disease and ulcerative colitis.
Infliximab works by blocking a molecule that promotes inflammation known as the tumor necrosis factor (TNF). High levels of TNF are considered to be a major sign of intestinal inflammation. When researchers introduced Infliximab into wells with an inflamed intestinal barrier, they observed that levels of TNF and other inflammatory molecules dropped off after 24 hours.
Building on preliminary results
Ultimately, the chip made for an easy-to-use and adaptable system. With the intestinal barrier established within a week, the researchers were able to observe interactions between immune and intestinal cells as well as test therapies. Moreover, the multiple wells of the chip allow different experiments to occur in parallel.
“With this system, we have not only been able to examine inflammation at the epithelial barrier but also to delve into the role of the intestinal subepithelial tissue in the development of inflammatory bowel disease,” said Nguyen. “This is a significant advancement, considering that such investigations, although highly valued […], have been challenging to conduct using existing intestine-on-chip systems.
“Nevertheless, our system will still need improvements to achieve the full level of biological complexity of a highly intricate in vivo intestinal microenvironment.”
The researchers hope that this chip will help add to the understanding of the underlying causes and pathology of inflammatory bowel disease, helping in the development of better therapies. Nguyen’s team also plans to work on similar models for the lungs, bladder, and placental tissue.
Reference: Oanh T. P. Nguyen, et al., A Versatile Intestine-on-Chip System for Deciphering the Immunopathogenesis of Inflammatory Bowel Disease, Advanced Healthcare Materials (2024). DOI: 10.1002/adhm.202302454
Feature image credit: Oanh Nguyen, et al.