There is no licensed vaccine available to protect against melioidosis, a tropical disease that kills around 89,000 people every year. Researchers are hoping to change this with a new vaccine candidate they’ve developed against B. pseudomallei, the bacterium that causes the disease.
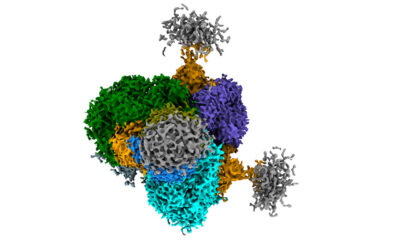
The new vaccine uses a modified version of a bacterium to safely deliver the molecules that trigger an immune response in the host’s cells. This “vector” is the same one employed in the development of successful vaccines against anthrax, the plague, and tularemia, also known as rabbit fever.
“The vector itself, called LVS delta capB […] is derived from a vaccine against tularemia known as live vaccine strain or LVS,” said Marcus Horwitz, professor of medicine and microbiology, immunology, and molecular genetics at the UCLA School of Medicine and senior author of the study.
Tularemia is a potentially fatal disease that usually affects rabbits, hares, and rodents but can also spread to humans. The original live vaccine strain contains a weakened form of a bacterium that causes tularemia.
While it offers some protection against infection, the vaccine is also toxic and can cause lymph node inflammation and pain at the inoculation site in up to 80% of those who receive it.
To address the problem of toxicity, the researchers removed a gene called capB, which resulted in more than 10,000 times less toxicity than the original vaccine. To create the melioidosis vaccine, they then inserted four specific B. pseudomallei genes that contain the instructions for making proteins that are known to trigger an immune response.
Protection against the most lethal form of melioidosis
Humans can contract melioidosis in a few different ways: by consuming water or food contaminated with B. pseudomallei, by exposure to the bacteria through a skin abrasion, or by inhaling contaminated airborne particles. “The respiratory route of infection with B. pseudomallei is considered to be the most lethal and the most difficult route to protect against,” Horwitz said.
To understand how well their vaccine protects against this route of infection, the researchers chose mice that are between 10 and 100 times more sensitive to B. pseudomallei than other research strains and immunized them by administering a small amount of the new vaccine into each nostril. The mice received three doses of the vaccine, each spaced four weeks apart. Then, four weeks after the last dose, they were exposed to a lethal dose of B. pseudomallei, also administered through the nose.
The researchers compared their results to a control group that received a “sham” immunization, but they also compared them to mice immunized with the new vaccine via an injection under the skin. Finally, to see how their vaccine held up against an existing vaccine, they compared the results to a control group they immunized with a melioidosis vaccine that is effective but considered unsuitable for use in humans.
Administering the vaccine through the nose was found to be more protective than conventional injection, even against high doses of B. pseudomallei. Mice that received the new vaccine in the nose had a median survival rate of 75% at 42 days; a separate experiment confirmed that even a single dose of the intranasal vaccine offered similar protection. When administered through the nose, the new vaccine was also as or more effective than the control vaccine.
Potential worldwide significance
Melioidosis infects thousands of people naturally, but it is also a Tier 1 Select Agent, which means health officials believe it has high potential to be used as a biological weapon.
“Availability of a safe and effective vaccine [against melioidosis] is important to global health security,” said Wesley Long, medical director of diagnostic microbiology at Houston Methodist Hospital, who was not involved in the study.
Long added that more work will need to be done before researchers will know if the vaccine is effective in humans. “At this point, all this work has been done in mice,” he said. “To move into humans, clinical trials first for safety and then for efficacy will have to be conducted and results in humans may vary from the results seen in mouse models.”
Before human trials can get underway, Horwitz said the vaccine needs to be tested for efficacy in a second animal model. “The Food and Drug Administration (FDA) requires this in the case of vaccines for which efficacy studies are otherwise not feasible,” he said. “If the vaccine does well in a second animal model, then it would be eligible for testing in humans for safety and immunogenicity.”
Additionally, Horwitz said the researchers would like to see if the vaccine can protect against an infection caused by contact with B. pseudomallei through a skin abrasion. They also plan to test it against a related bacterium called B. mallei.
“This pathogen causes glanders in humans and animals and is also a Tier 1 Select Agent of bioterrorism,” said Horwitz. “B. mallei contains some of the same antigens expressed by our vaccine.” If the vaccine also shows promise in these studies, it could go on to play a role in protecting against not one but two important diseases, potentially saving thousands of lives.
Reference: Marcus Horwitz, et al., LVS ΔcapB-vectored multiantigenic melioidosis vaccines protect against lethal respiratory Burkholderia pseudomallei challenge in highly sensitive BALB/c mice, mBio (2024), DOI: 10.1128/mbio.00186-24
Feature image credit: Sandy Millar on Unsplash