There are “four pillars” of cancer treatment: Surgery, radiation, chemotherapy, and immunotherapy. No one of these therapies works for everyone, and a patient’s progress can be slowed or halted by drug resistance.
Cancer cells can become resistant to nearly every kind of conventional treatment, which means a drug that seemed life-saving may just stop working, sometimes within weeks of starting treatment. This is why it’s impossible to predict which patients will do well and which will not.
A team of researchers at Rice University in Texas hopes to introduce another pillar of treatment to help improve patient outcomes: mechanical therapy, which could overcome the problem of treatment resistance.
Destroying cancer cells with vibrating molecules
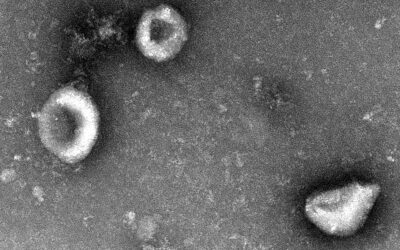
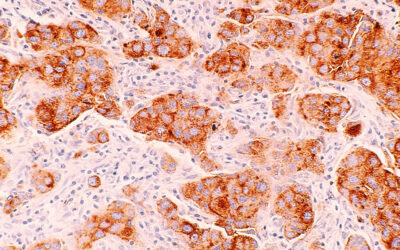
Led by Ciceron Ayala-Orozco, the team has found a way to destroy cancer cells using a type of molecule called a cyanine. Cyanines are probably best known for their medical uses; synthetic cyanine dyes are FDA-approved for applications such as tracing blood flow in the human body and identifying tumors.
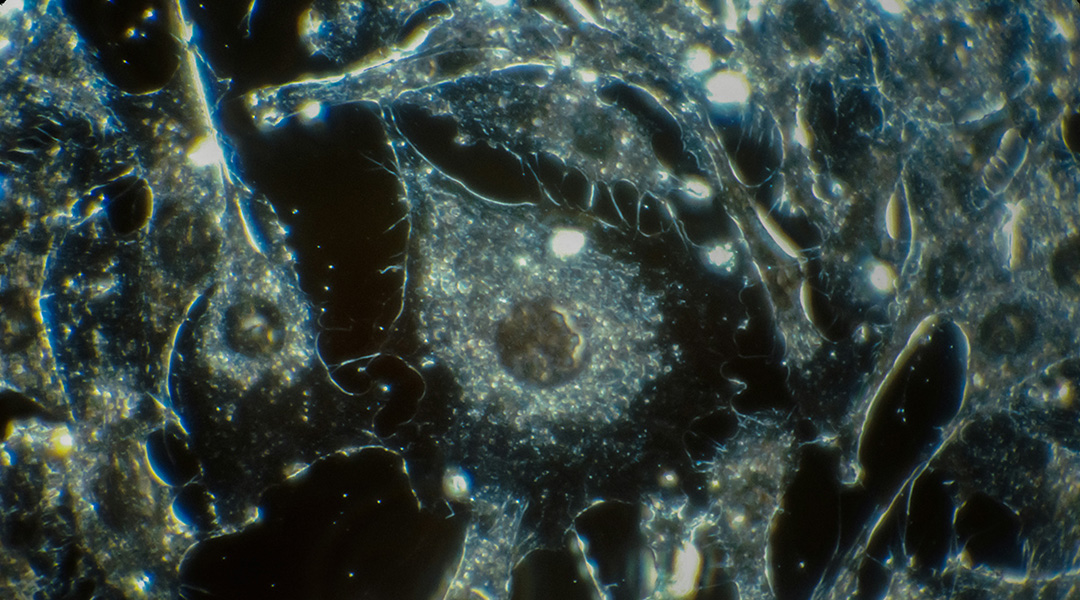
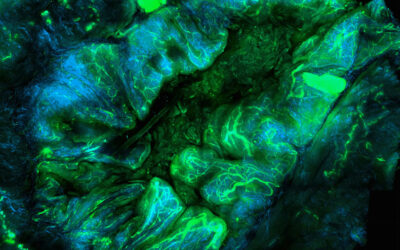
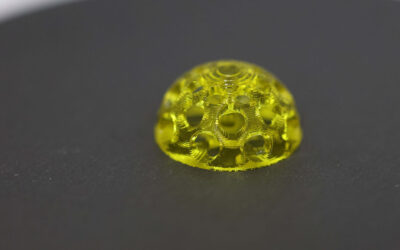
The Rice University researchers discovered that cyanine dyes vibrate at up to 40 trillion oscillations per second when exposed to near-infrared light. “Anything that is surrounded by the molecules will be disassembled very quickly,” said Ayala-Orozco. “You can literally see the cell shaking and breaking, making holes in this membrane. You can see there is a hole made immediately within minutes.”
Key to this discovery is that the cells are destroyed by mechanical action rather than by photothermal or photochemical action. “This is not any type of vibration in the molecule,” Ayala-Orozco said, “but a unique type of whole-molecule vibration.” The researchers call this the “molecular jackhammer” effect.
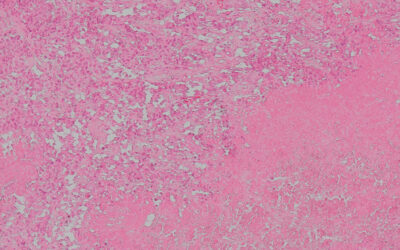
When Ayala-Orozco and his co-authors tested the molecular jackhammer on human melanoma cells they were able to destroy 100% of them. Once fully developed, they believe this therapy could be used without concern for resistance since it is impossible for cancer cells to develop resistance to mechanical destruction.
During certain procedures, surgeons need a light source to help visualize the tumor and surrounding tissues. This means a therapy that uses near-infrared light wouldn’t be significantly different from some of the techniques already being used. “There are a lot of oral cancers where we can introduce a fiber optic through the oral cavity,” Ayala-Orozco said. “In bladder cancer, doctors already introduce optical fibers to observe inside the bladder and even treat some cancers.”
The use of near-infrared light is an important feature as other types of light, like visible blue light, can’t bypass the top layer of human tissue. “The penetration they have is very shallow, maybe one millimeter or less,” Ayala-Orozco said. “With near-infrared light we can go two centimeters.”
Sunil Krishnan, a professor of radiation oncology at UTHealth Houston who was not involved in the study, said the use of near-infrared light has benefits beyond just giving surgeons the ability to reach deeper tissues and organs.
“Needless to say, non-specific activation in non-target normal cells needs to be averted,” he said. “Another advantage of being outside the typical visible light window is that spontaneous unintended triggering of jackhammer action by white light, even before laser illumination, could be reduced.” Krishnan added that the molecular jackhammers might also need to be targeted to specific parts of the cancer cell to avoid killing healthy cells.
Where will mechanical cancer therapy be used?
Ayala-Orozco believes the treatment could have a few different applications, for example, a surgeon could use it to remove stray cancer cells after a large tumor has been surgically removed. It could also be used to treat cancers that can be accessed laparoscopically, such as GI cancers.
Ayala-Orozco said the therapy could even kill disease-causing microorganisms, such as bacteria and fungus, particularly those that cause localized infections. “There are some cases of toenail infection that are very hard to treat,” he said, “so this could be one option.”
Because this particular study only tested the therapy on melanoma cells, Ayala-Orozco said there has been some criticism. Melanoma, a type of skin cancer, is already relatively easy treat, provided it’s caught in the early stages. If this therapy proved to only work on skin tumors, it wouldn’t have many advantages over excision, the usual treatment for early-stage melanoma.
This means the team needs to prove their therapy can work on other types of cancer such as pancreatic cancer, which tends to be aggressive and difficult to treat. “The next step is to do a lot of work in vivo with mice,” Ayala-Orozco said.
Like any new potential cancer treatment, the molecular jackhammer will have to prove itself and get through the development and approval process before it will be an option for patients. If it does, this new pillar of cancer therapy could represent hope for patients who may one day face treatment-resistant disease.
Reference: Ciceron Ayala-Orozco, et al., How to Build Plasmon-Driven Molecular Jackhammers that Disassemble Cell Membranes and Cytoskeletons in Cancer, Advanced Materials (2024). DOI: 10.1002/adma.202309910
Feature image: National Cancer Institute