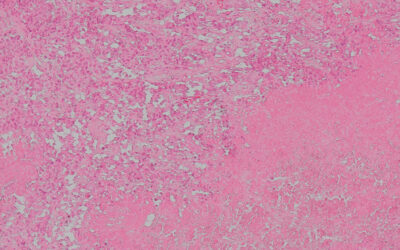
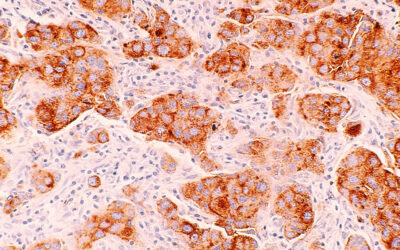
Researchers have identified a molecule that plays a key role in the spread of cervical cancer to other tissues, a process known as metastasis — a challenge to prevent. Their work has revealed a new approach to treating cervical squamous cell carcinoma, which accounts for up to 80% of cervical cancers.
This form of cancer typically spreads to the lymph nodes located near the bottom of the spine, making it more challenging to successfully treat the cancer.
“The lymph node is the most common site of distant metastasis of cervical squamous cell carcinoma,” stated the authors of the study published in Advanced Science. “The presence of lymph node metastasis itself decreases the 5-year survival rate from 95% to 33.3%.”
RNA could be the culprit
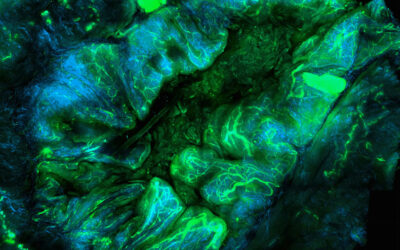
The researchers set out to find new drug targets for these patients, who currently lack any therapies that specifically target the spread of their tumors. In particular, they looked at the molecules that drive the growth of lymphatic vessels, a process that enables cancer cells to spread to the lymph nodes.
What they found was a circular RNA molecule that they named LNMAC, short for lymph node metastasis associated circular RNA. “Lymph node metastasis is a complicated biological process,” the scientists stated. “Accumulating evidence indicates that circular RNAs may be involved in metastasis of many cancers including bladder, lung and cervical [cancer].”
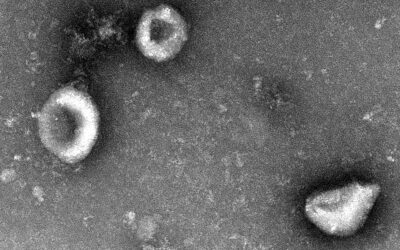
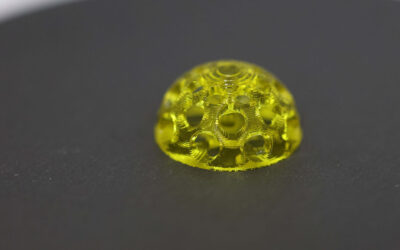
Circular RNA has a very similar structure to messenger RNA, which is well-known for being the basis of several COVID-19 vaccines. But unlike messenger RNA molecules, which are linear, circular RNA molecules form a loop (hence the name) that protects them from being broken down inside the cell.
Looking at samples from cervical tissue, the researchers found that patients with metastatic cervical squamous cell carcinoma had higher levels of LNMAC compared to healthy people. The higher the levels of this molecule, the shorter the overall survival of the patients.
Targeting cervical cancer metastasis
The researchers then took to mice to investigate the exact mechanism by which LNMAC causes metastasis to the lymph nodes. Their results revealed that LNMAC controls the metastasis process by relying on epigenetics, which consists of altering the activation or deactivation of specific genes without altering their DNA code.
More concretely, LNMAC activates the genes that encode a protein called FGF2, a growth factor that among many other functions is responsible for forming new blood and lymphatic vessels.
Epigenetic drugs have been tested in clinical trials as potential cancer drugs, but so far they have achieved limited results and caused serious side effects. The results from the study highlighted a possible reason why, as the researchers noted that certain epigenetic drugs can actually activate the genes encoding for FGF2.
“Caution should be exercised when using [them] as anticancer drugs in tumors prone to lymphatic metastasis, especially cervical squamous cell carcinoma,” they wrote.
To get around this challenge, they opted for a different strategy consisting of directly targeting and blocking the FGF2 protein using antibody drugs. In mice, this strategy was successful at preventing lymph node metastasis by blocking the effects of LNMAC and inhibiting the formation of new lymphatic vessels.
“It is becoming evident that the effects of FGF2 on tumor [lymphatic vessel growth] are far more important than previously assumed,” the scientists stated. They believe that preventing the growth of lymphatic vessels by targeting FGF2 has potential to be an effective treatment for patients with metastatic cervical squamous cell carcinoma.
Further tests and eventually clinical trials will have to confirm these findings before cancer patients can benefit from this new strategy. If successful, this research could bring hope for a large group of cancer patients that currently lack effective therapies.
Chunyu Zhang et al., LNMAC Promotes Cervical Squamous Cell Carcinoma Lymphatic Metastasis via Epigenetic Regulation of FGF2-Induced Lymphangiogenesis, Advanced Science (2024). DOI: 10.1002/advs.202404645
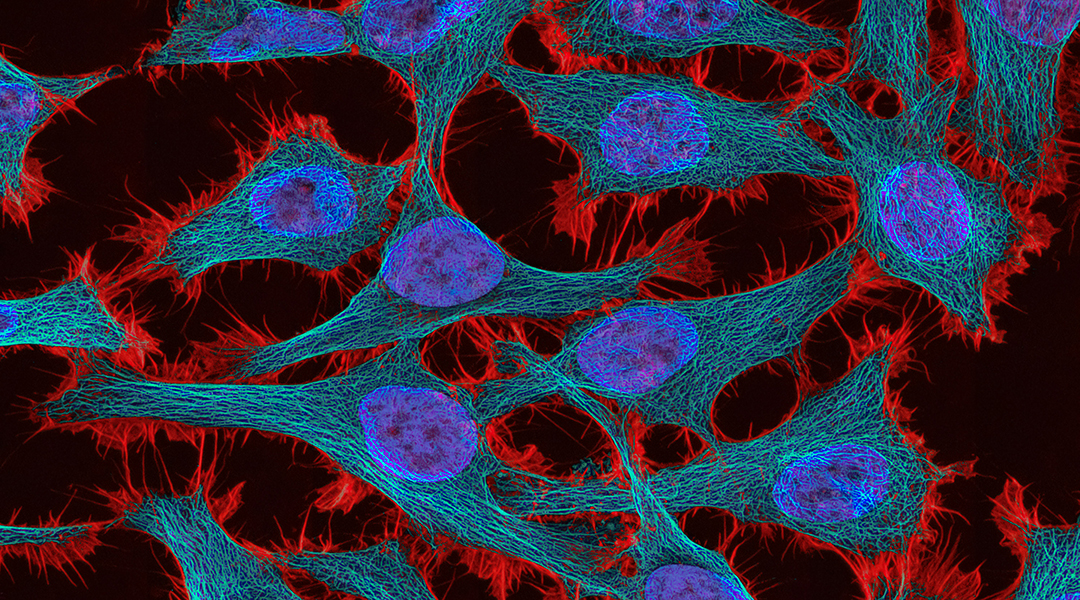
Feature image credit: National Cancer Institute