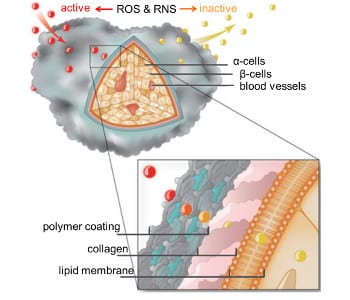
Polymer coating protects pancreatic islet cells by deactivating inflammatory reactive oxygen (ROS) and nitrogen species (RNS).
Type 1 diabetes is an autoimmune-mediated disease resulting in the destruction of insulin-secreting pancreatic β-cells. As a result of insulin deficiency, numerous complications including cardiovascular disease, nephropathy and retinopathy may ensue and diminish the quality of life of the patient.
The use of exogenous insulin is vital for maintaining normal blood glucose levels and transplantation of insulin-producing cells is considered the most reliable strategy to achieve in vivo glucose control. However, the clinical application of pancreatic islet cell transplantation remains limited due to the use of toxic immunosuppressive therapies to prevent immune-mediated rejection.
To overcome these complications, the Kharlampieva and Tse research groups at the University of Alabama at Birmingham have developed a nanothin anti-inflammatory polymer material capable of decreasing immune responses involved in islet transplantation rejection. The material consists of hollow macroparticles (capsules) with nanothin shells of hydrogen-bonded multilayers of natural polyphenol (tannic acid) and a neutral polymer.
These capsules successfully scavenge noxious reactive oxygen and nitrogen species as well as significantly attenuate the production of pro-inflammatory cytokines. The ability of tannic acid-containing capsules to diminish the synthesis of these immune-mediated inflammatory molecules demonstrate great promise in preventing transplantation rejection.
When applied to living pancreatic islet cells, this material has the potential to physically protect transplanted cells and prevent undesirable immune responses. Ultimately, Type 1 diabetics will regain a lifestyle independent of exogenous insulin administration and maintenance of proper glucose homeostasis.